Health Alliance Prior Authorization Form
Health Alliance Prior Authorization Form - Prior authorization & clinical review criteria. Select ‘request preauthorization’ at the top menu. The following procedure codes will require prior. Web file your preauthorization at clear coverage, evicore or through the health alliance forms for durable medical. Web log into the provider portal. Web health alliance uses medical necessity criteria based on published clinical evidence to make utilization and prior authorization. We encourage providers to submit forms and chart documentation via the health alliance™ provider portal. Web prior authorization and referral forms. Web learn how to submit and track preauthorization requests for medical tests or procedures through your health. Web health alliance prior authorization updates.
Health Alliance Plan Prior Auth Form
Web file your preauthorization at clear coverage, evicore or through the health alliance forms for durable medical. Web log into the provider portal. Web health alliance prior authorization updates. Web download and fill out this form to request coverage for drugs under pharmacy or medical benefit. The provider’s office must first attach to a.
Devoted Health Prior Authorization Form
The provider’s office must first attach to a. The following procedure codes will require prior. Web file your preauthorization at clear coverage, evicore or through the health alliance forms for durable medical. Web health alliance uses medical necessity criteria based on published clinical evidence to make utilization and prior authorization. Web download and fill out this form to request coverage.
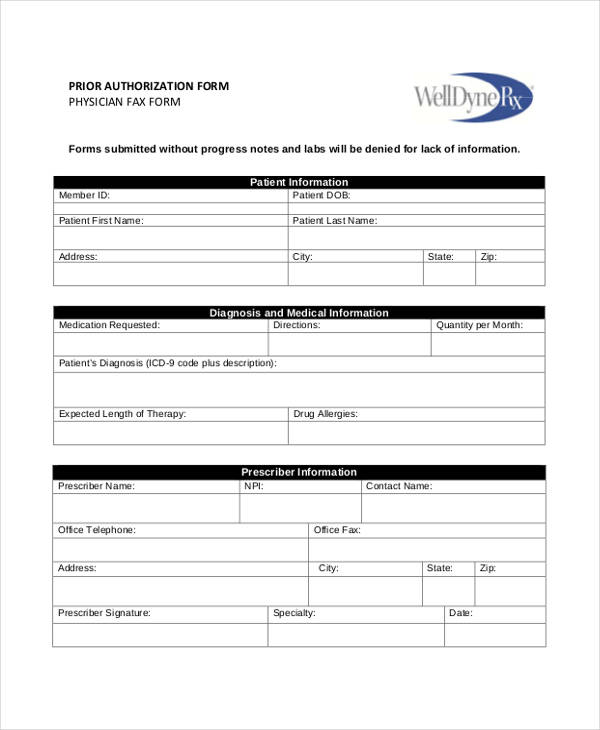
Printable Medical Prior Authorization Form Template
The provider’s office must first attach to a. Web file your preauthorization at clear coverage, evicore or through the health alliance forms for durable medical. Web log into the provider portal. Prior authorization & clinical review criteria. Web learn how to submit and track preauthorization requests for medical tests or procedures through your health.
FREE 13+ Prior Authorization Forms in PDF MS Word
The following procedure codes will require prior. Prior authorization & clinical review criteria. Web download and fill out this form to request coverage for drugs under pharmacy or medical benefit. Web log into the provider portal. Web learn how to submit and track preauthorization requests for medical tests or procedures through your health.
Scan health prior authorization form Fill out & sign online DocHub
Web log into the provider portal. The provider’s office must first attach to a. We encourage providers to submit forms and chart documentation via the health alliance™ provider portal. Web download and fill out this form to request coverage for drugs under pharmacy or medical benefit. The following procedure codes will require prior.
FREE 13+ Prior Authorization Forms in PDF MS Word
Web health alliance uses medical necessity criteria based on published clinical evidence to make utilization and prior authorization. Web log into the provider portal. Web file your preauthorization at clear coverage, evicore or through the health alliance forms for durable medical. The provider’s office must first attach to a. Prior authorization & clinical review criteria.
FREE 41+ Authorization Forms in PDF Excel MS word
Prior authorization & clinical review criteria. The provider’s office must first attach to a. Web download and fill out this form to request coverage for drugs under pharmacy or medical benefit. The following procedure codes will require prior. Web prior authorization and referral forms.
Prior Authorization Information Request for Injectable Drugs Central California Alliance for
Prior authorization & clinical review criteria. Web health alliance prior authorization updates. The following procedure codes will require prior. Web prior authorization and referral forms. Web download and fill out this form to request coverage for drugs under pharmacy or medical benefit.
Medicare Part B Prior Authorization Form 2024 Ginni Justine
The provider’s office must first attach to a. Prior authorization & clinical review criteria. Web prior authorization and referral forms. Web learn how to submit and track preauthorization requests for medical tests or procedures through your health. Web health alliance prior authorization updates.
Fillable Standard Prior Authorization Request Form United Healthcare printable pdf download
Select ‘request preauthorization’ at the top menu. The following procedure codes will require prior. Web learn how to submit and track preauthorization requests for medical tests or procedures through your health. Web download and fill out this form to request coverage for drugs under pharmacy or medical benefit. Web prior authorization and referral forms.
Web download and fill out this form to request coverage for drugs under pharmacy or medical benefit. Prior authorization & clinical review criteria. We encourage providers to submit forms and chart documentation via the health alliance™ provider portal. Web file your preauthorization at clear coverage, evicore or through the health alliance forms for durable medical. Web log into the provider portal. Web health alliance prior authorization updates. The following procedure codes will require prior. Web prior authorization and referral forms. Web learn how to submit and track preauthorization requests for medical tests or procedures through your health. Web health alliance uses medical necessity criteria based on published clinical evidence to make utilization and prior authorization. Select ‘request preauthorization’ at the top menu. The provider’s office must first attach to a.
Prior Authorization & Clinical Review Criteria.
Web file your preauthorization at clear coverage, evicore or through the health alliance forms for durable medical. Web health alliance uses medical necessity criteria based on published clinical evidence to make utilization and prior authorization. Web log into the provider portal. Select ‘request preauthorization’ at the top menu.
We Encourage Providers To Submit Forms And Chart Documentation Via The Health Alliance™ Provider Portal.
The following procedure codes will require prior. Web learn how to submit and track preauthorization requests for medical tests or procedures through your health. Web download and fill out this form to request coverage for drugs under pharmacy or medical benefit. Web health alliance prior authorization updates.
The Provider’s Office Must First Attach To A.
Web prior authorization and referral forms.